Treatment of an infantile scoliosis using a ScoliBrace
Female patient aged 3 years with an infantile scoliosis.
Summary:
This case demonstrates the successful treatment of a moderate sized infantile scoliosis using a ScoliBrace rigid orthosis in a 3-year-old female patient. The patient’s scoliosis had initially been picked up by a GP who then referred the patient to an orthopaedic surgeon. The surgeon prescribed bracing and the child was issued with a rigid TLSO made by a hospital orthotist.
Unfortunately, the child’s scoliosis was still significant (33° in-brace) despite wearing the orthosis correctly. The parents of the child were concerned and sought a second opinion. The child was examined at the clinic and prescribed a 3D over-corrective ScoliBrace rigid orthosis. A complete resolution of the scoliosis could be obtained in-brace with the new orthosis.
The child wore the ScoliBrace for 24 months which resulted in a reduction of the curve from 40° down to 14°. The child is still under care and will continue with a soft-brace to encourage the correction of the remaining deformity as the child grows.
Case Background
The 3-year-old female patient presented to the clinic with postural deformity and lateral shifting of her trunk. The deformity had been picked up by the child’s parents who had then consulted with a GP.
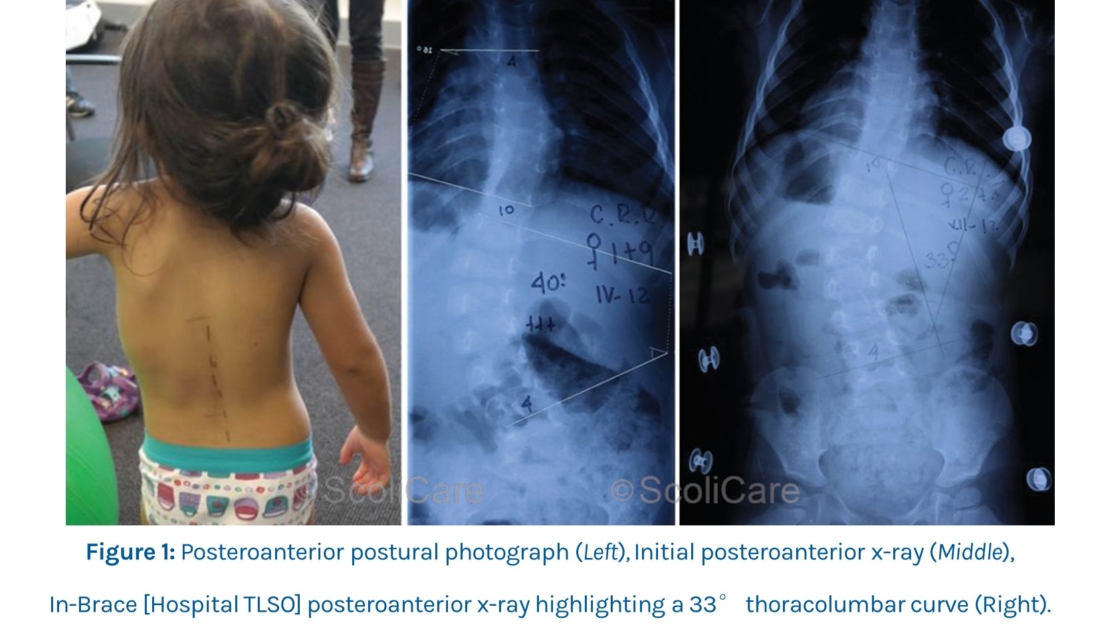
X-ray imaging ordered by the GP revealed a left thoracolumbar curve measuring 40° and a mild (10°) compensatory right thoracic curve (Figure 1). The GP had made a diagnosis of infantile scoliosis and referred the patient on to an orthopaedic surgeon for an appraisal.
After assessing the patient and reviewing the x-rays, the surgeon suggested that bracing would be the most suitable treatment in this case.
The patient was subsequently issued with a rigid brace (thoraco-lumbo-sacral orthosis [TLSO]) that had been designed and fitted by the hospital orthotist.
In-brace x-rays taken soon after the TLSO fitting showed a reduction in the size of the primary curve from 40° to 33° (Figure 1). While a reduction in the curve was evident, the parents of the patient had concerns that there was still significant deformity present despite wearing the TLSO. This prompted them to seek a second opinion from the xlinic.
Examination Findings
The history and physical examination performed at the clinic aligned with the findings from the previous imaging results.
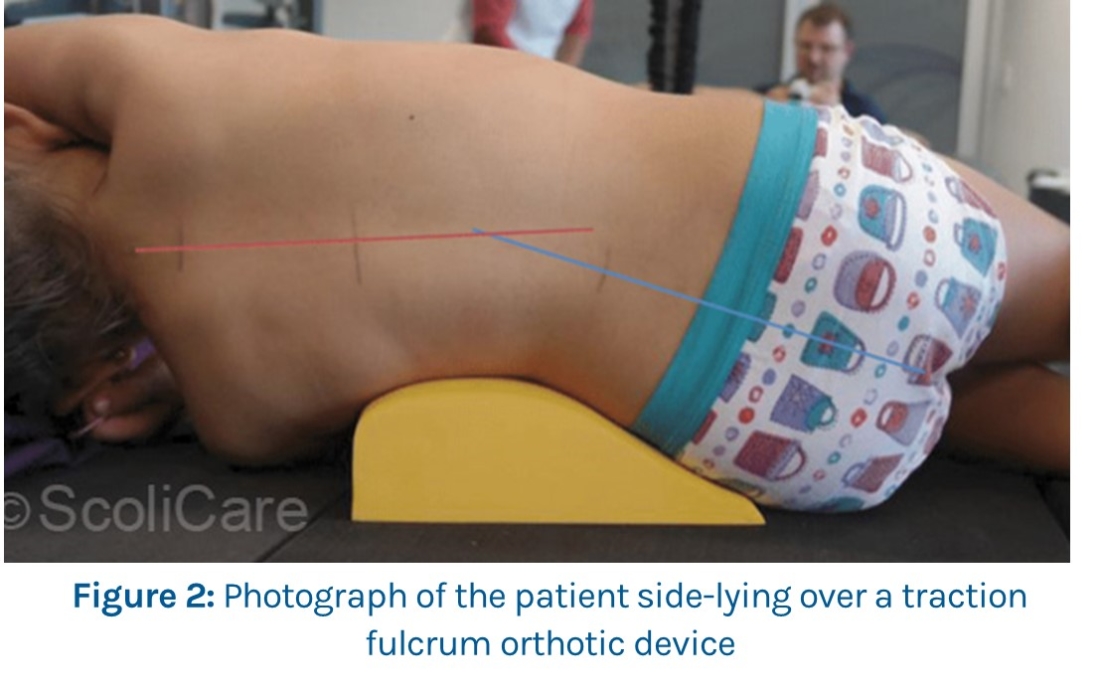
The patient’s trunk was significantly translated to the left during both the postural and gait analyses, without evidence of leg length discrepancy or pelvic anomaly. The primary curve appeared flexible (Figure 2) which was a favourable sign for brace therapy.
Intervention
A new custom ScoliBrace was prescribed for the patient along with some home-based stretching and exercises to help with the abnormal trunk shift.
The patient was advised to wear the brace full-time (up to 23 hours per day) and perform the rehabilitation exercises daily.
Outcomes
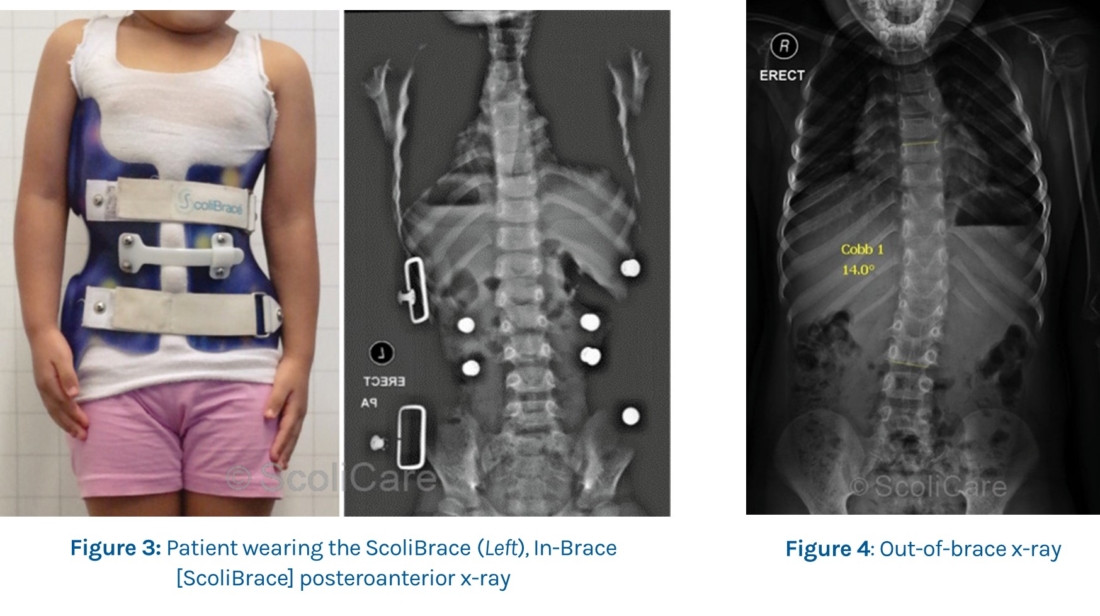
In-brace x-rays taken at the time of the brace fitting revealed that the deformity could be completely reduced (Figure 3). The patient continued to wear the brace with good self-reported compliance from the parents.
Unfortunately, the daily exercises were performed on a more haphazard basis. ScoliBrace treatment was continued for approximately 24 months.
Several modifications were made to the brace along the way to accommodate the patient’s growth.
By the end of the bracing period, the patient’s scoliosis had been reduced from 40° down to 14° out of the brace (Figure 4).
At this point in time the patient is still under care, however the recommendation is for the patient to wear a more flexible style brace to maintain the correction achieved with the ScoliBrace, and also to further reduce the left postural shift.
Discussion
This case highlights the management of an infantile idiopathic scoliosis (IIS) case using a ScoliBrace orthosis.
Patients with IIS typically present before the age of 3 years and are classified into two categories – resolving and progressive. Curves in patients with the resolving type tend to reduce spontaneously over time, whereas curves in patients with the progressive type continue to worsen leading to crippling deformity and reduced quality of life if not treated.
Casting is typically initiated before the age of two years in these patients as it is more difficult to attain a complete resolution of the deformity if treatment is initiated after this point. After a significant result has been obtained with casting, the patient is usually placed into a rigid brace to stabilise the correction.
There are unique features to this particular case. Thoracolumbar presentations are less common compared to thoracic presentations in IIS patients, and the presence of compensatory curves is also somewhat unusual in this population.
In this case, bracing has been used as a first-line management approach versus the more traditional approach involving serial casting. The patient’s initial hospital-made-brace was substandard as evidenced by the small (17.5% reduction) in-brace correction, and had the patient continued with this brace it is likely that the curve would have continued to progress.
At this point in time the evidence to support the use of bracing as a primary treatment in patients with IIS is sparse, however the results observed in this case would suggest that a more comprehensive investigation of ‘over corrective’ 3D bracing such as the ScoliBrace, is justified.
Conclusion
This case demonstrates the reduction of a severe thoracolumbar scoliosis in a young child using a ScoliBrace orthosis.
NB: Results vary from case to case. Our commitment is to recommend the most appropriate treatment based on the patients type and severity of scoliosis.
© ScoliBrace
